Jambo from Siaya, Kenya! The new ‘mzungu’ (white person) has arrived in town. My first discovery about the Kenyan people is that they are very friendly and have super human seeing capacity. They can spot a mzungu from literally miles away. All I hear is a faint “mzungu, mzungu!!” and someone will be waving furiously in the distance. Or maybe I stick out more than I realized, given I haven’t seen a fellow mzungu since I arrived. After only a few days, passing taxi drivers started yelling “to Ulamba?” (the orphanage where I am staying) before I could even open my mouth…very convenient really.
My trip here went very smoothly. After a short flight from a busy, relatively advanced Nairobi, I arrived in the quieter, dusty Kisumu on the shores of the huge Lake Victoria, the third largest fresh water lake in the world. I was met at the airport by a member of my new Kenyan family, Odongo, who helped me and my bag on to the local transport, “matatus” which are taxi vans.
If you ever wondered how many full grown Kenyans and New Zealanders you can fit in a van, I now have the answer. A lot. If another four hang half in, half outside the van, the total gets well in to the mid 20’s. And just when I thought we must surely be at capacity, one more squeezes in the driver’s seat with the driver hopping back in to steer the vehicle, from on top of the passengers knee. Hakuna matata.
This is my mode of transport to and from Siaya Hospital every day. I love it, because it guarantees at least a bi-daily entertainment fix. I cannot help but laugh at the creativity to fit one more person in! I would love to get a photo but unfortunately once I’m sandwiched in there is no hope of me moving my arms to take one.
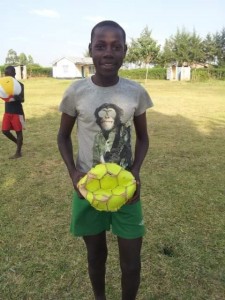
My accommodation is at Ulamba Orphanage, 20min drive from Siaya Hospital and the main town. There are 32 children living here ranging from 2 to 18 years, two cats, two cows, two goats and lots of chickens, doves and insects. Since I arrived there has been a teacher’s pay strike so that means, in between chores of course, there is lots of soccer to be played.The orphanage is run by delightful Mama Rose, who instantly acquired her 33rd child when I arrived. She is quick to pull your leg, as are most Kenyans. I got very excited when she told me to watch that I didn’t burn myself in the shower, I couldn’t believe I had access to a hot water. When I gave it a whirl, it was to say the least, refreshing! I have also been greatly expanding my cooking repertoire with the children’s help, by learning to cook Kenyan style.
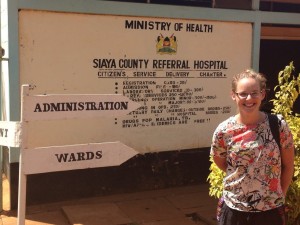
My working placement is at Siaya County Hospital. It is a 220 bed hospital with a catchment population of nearly a million people. It has three consultant doctors. Only one is a resident, the other surgeon and physician are shared with other hospitals in the county.
There are five medical officers (more junior docs), eight interns (equivalent of me), 55 nurses, nine clinical officers (specialist nurse) and a heap of trainee nurses from the medical school beside the hospital. How is that for a patient load?!
It offers a huge range of services. Obstetrics, gynaecology, general medicine, family medicine, orthopaedics, oncology, paediatrics, specialist HIV and malaria clinics, physio, OT, dental, labs, a research centre used by the CDC, pharmacy, physiatric services, palliative and end of life care, mortuary and embalment.Most patients attend hospital as the first port of call for medical care as there are no such thing as community doctors here. Out in the community there are nurse run Dispensaries and volunteer run Health Posts which can provide a basic level care only. The rest are referred to hospital. It was a huge surprise for the student nurses I have been working with to learn New Zealand has consultant GPs providing primary care in the community when here, they struggle to track down doctors within their own hospital.
To start, I have been working in Women’s and Child’s Health and Family Planning. I am over the moon about this as one of my goals of this trip was to learn how the care and health of women and their babies was managed, as the next generation of society. They have a definite focus on providing services to HIV positive mothers which has been very interesting within a context of poverty and limited resources. They have been fantastic in involving me in giving malaria, BCG and polio vaccinations, doing HIV testing on women and babies, giving family planning advice, diagnosing simple complaints like shingles and taking cervical smears.
The PMTCT (Prevention of Mother To Child Transmission) clinic has been one of my favorites. This is for HIV positive mothers and their new born children. It is extremely busy with patient after patient until finishing up time. Siaya has one of the highest prevalences of HIV in Kenya, 19% in the population and 9% of pregnant women. There are multiple historical reasons for this. Firstly when HIV was starting to take hold in Africa it was common practice that if a man died his brother would receive his wife. Further, witch-doctors were commonly used and touted miracle cures for HIV. People believed in their practices, in the mean time continued customary ways which aided the spread of the virus. They have also trialed needle exchange programs but these unfortunately were short lived due to lack of money and resources to keep up with the demand, so needle sharing continued.
Pregnant women are screened for HIV in the first and third trimester through an opt-out system. Women diagnosed as HIV positive are given counseling and support to reduce the chance of transmission to their baby. HIV positive women give birth normally and breast feed their babies as c-sections and infant formula is too expensive for almost all women to afford. The current mother to child transmission rate here is 3%.
Mothers are encouraged to breastfeed exclusively for at least the first 6 months. Mix feeding with cows milk and millet porridge increases infant mortality rate and the chance of the baby acquiring HIV by exposing the baby to infection causing bacteria and parasites which damage the gut lining increasing opportunities for HIV to reach the blood stream. The babies are started instantly from birth on anti-retroviral treatment (ART) prophylaxis and an antibiotic syrup to prevent opportunistic infections.
At 6 weeks, babies are first tested for HIV which happens in this clinic. They are also tested at 9 months and 18 months and if found to be positive at any of these points they are started on life long ART. If tests are negative they are discharged after 18 months. It really is a mixed bag of emotions in these clinics. The expression on mother’s faces when their baby is declared HIV negative at 18months cannot be explained. It is a look of overwhelming joy and relief. In contrast, a diagnosis of HIV can be devastating. One young mum with a HIV positive 6 week old swore she would never have another child and could not understand why her second baby has HIV and her first born didn’t, even though she had never missed taking her medication.
Fortunately all HIV medication and care is free and funded by the American Government. HIV positive women must come to hospital (which can be any hospital in Kenya) monthly for their prescriptions. As you can imagine is quite an expensive task for those who live some distance away. A notable barrier to full adherence. The team here are doing a great job. Many of the support staff are HIV positive mothers and a real effort is made to support these women is a very caring environment.
At 6 weeks post partum, women are encouraged to attend the family planning clinic and start on long-term contraception, either Intrauterine devices (IUD’s) or hormone releasing rods which are inserted with local anesthetic under the skin in the upper arm, offering contraception for 3-5 years. Long term options are encouraged as it dramatically reduces patient load for family planning services if they don’t have to return for a contraceptive pill prescription every 3 months as well as being a highly effective means of preventing pregnancy. Again this contraception is totally free to all women through USAid.
The student nurses here are incredibly skilled and hands on, the consequence of a lack of employed man-power to cope with the patient load. Before they have even graduated, they are doing things we would only do in New Zealand with specialist training. They have taken me under their wing and shown me how to insert contraceptive devices. After watching one it was my turn, so with shaking hands they walked me through it. By the end of the day I had inserted 8 and was offering to do any that walked through the door. I have added a great clinical skill to the tool belt.
Some women are reluctant for these methods and desperately want to use ‘the pill’. Apparently it is common for new mothers to buy the estrogen containing contraceptive pills from local dispensaries. While trying to protect themselves, they are unaware oestrogen containing pills are contraindicated for breast feeding women. Consequently milk production drops and mothers wean babies very early before 3 months of age. One disadvantage of having uncontrolled dispensing of medicine.
I have also attended palliative care clinics which are certainly an eye opener and a fascinating insight in to mechanics of Kenya’s health system. The patients are often shuffled from health professional to health professional, department to department at significant expense, time, stress and frustration without an answer for their symptoms.
“Presumed cancer” is a buzz word here much to the frustration of the oncologist. There are not the sophisticated CT, MRI and diagnosing techniques we have access to and in many cases treatment may be initiated without a diagnosis. Simple, low cost methods are used for ‘diagnosis’ such as ultrasound, x-ray, blood markers especially PSA for prostate cancer, visualization for cervical cancer and in many cases clinical suspicion. One patient had both testicles removed last year and still doesn’t have a definitive diagnosis of prostate cancer. This surgery was organized based on a moderately raised PSA. The reason for the surgery was that prostate cancer cells often “feed” off testosterone produced by the testes.A patient may have a biopsy if they can afford it and get themselves to a center with a pathologist, to analyse the sample works. The next problem is the results take literally months to be reported – six months in the case of one women with cervical cancer. Chemotherapy treatment can be administered in Siaya. Radiotherapy requires a trip to Nairobi and the waiting list is so long patients are waiting a year for treatment. Although subsidized by the government all cancer treatments cost. This causes further delays while the patient saves or gathers enough money for treatment from family and friends.

Eating traditional maize ugali, hands and all, the suspected culprit of high rates of oesophageal cancer in this area.
The next most prevalent cancer is cervical, prostate, karposi sarcoma and breast cancer. Karposi Sarcoma is a cancer which effects immunocompromised HIV patients. It is suspected the cancer rate is much higher than what is seen at the hospital clinics with many people dying at home. It is not realised that the patient has cancer but rather the patient and family just accept the person is sick and their time is up.
Presentations are most often late in the disease course. One HIV patient I saw had a fungating, seeping penile cancer the size of baseball, which he had wrapped in a tiny piece of dirty cloth as a dressing to try and protect his clothes. He had presented 2 years ago with a sore on his penis. He was given antibiotics and that was the last time he has sought medical help despite attending the hospital every month for HIV medication. In the mean time it has grown and grown and now consumes his whole penis with only the very tip recognizable as normal skin. Lymph nodes were extensively involved in the inguinal region and could be visualised easily without having to palpate. It must be heart sinking for the oncologist when these cases reveal themselves. It certainly was for me.
After a rather extended first blog, I’ll look forward to writing my experiences next week from behind a surgical mask. Tutaonana baadaye – see you later.


No comments yet.
Leave a comment